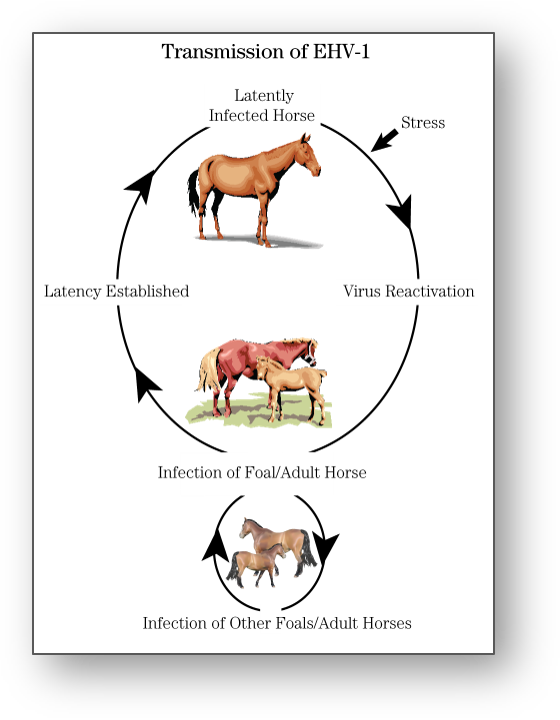
In certain regions of the world outbreaks of EHM appear to be increasing in frequency over the past 25 years. EHM is caused by Equine herpesvirus 1, a virus responsible for upper respiratory infections, late-term abortion, death in newborn foals, as well as spinal cord disease. There is neuropathogenic variant of EHV-1, which leads to higher viraemic load and greater nasal shedding. Most infections begin when horses that are latently infected experience a period of stress, leading to virus recrudesce. The neuropathogenic strain of EHV-1 is highly contagious. Unfortunately, EHM is associated with high mortality, around 40%, but this can be higher in some outbreaks. The neurologic form, EHM, is a devastating disease and it is only a matter of when, not if, outbreaks will be seen in Australia.
What are the signs of EHM
The signs typically begin 6 to 10 days after infection. An episode of cough and nasal discharge often occur within 2 weeks of neurologic signs. Fever is also a predictor of neurologic signs, although not all febrile horses will go onto develop spinal cord signs. The neurologic signs typically begins after the fever ends. These signs typically progresses rapidly before stabilizing. There is an ascending paralysis that begins in the rear limbs (paraparesis) and moves forwards to sometimes involve the forelimbs (tetraparesis). Urinary incontinence is common, along with cauda equina signs.


Diagnosing EHM
The diagnosis can be confirmed by requesting a PCR test on a nasal swab or blood sample (buffy coat). Collection of cerebrospinal fluid (CSF) is very helpful as samples are typically yellow. This is called xanthochromia. CSF protein levels are increased, although cell counts are typically normal.

Management and Prevention
Nursing care is critical. Some horses are unable to stand and therefore slinging becomes important. It is also important to protect the bladder through catheterization. Non-steroidal drugs (flunixin) and antioxidants (Vitamin E) are indicated. Corticosteroids are highly controversial. Antivirals, aspirin, heparin and pentoxifylline are also often used. The prognosis for EHM horses is guarded for survival.

Vaccines are not directly protective against EHM although they may reduce the magnitude and the duration of virus shedding in diseased horses. Zinc may be protective.
Biosecurity is critical to prevent spread. A case at a show, or at a boarding facility, or veterinary hospital has major implications for other horses that are co-located. Horses need to be isolated, tested and monitored for fever.
Tags: Infectious diseases; Neurology
